This post was written by Tabitha Morgan, an undergraduate student majoring in gerontology.
What is Medicare?
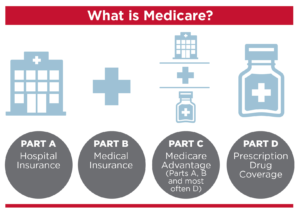
Medicare is a health insurance system that is through the government that is offered to those who are 65 years and older, people who are living with disabilities, and people with ALS or End-Stage Renal Disease. This form of health insurance has four parts, and each part covers different aspects of healthcare. The first one is Part A, which covers hospital stays, nursing home stays, and it also helps cover hospice care and some home health benefits that will be discussed. Next is Part B, this section covers doctor visits, outpatient care, services to help prevent diseases and illnesses along with help covering some medical supplies. Then there is Part D, which helps cover prescription medications. There is also a Part C which is a combination of parts A, B, and D¹. Within Medicare there is what is called the Home Health Benefit, which will be broken down and discussed next.
Home Health Benefit and What it Means
Home health care is when someone is in need of medical services and cannot leave their home or find it more comfortable to receive care at home. The following services may be eligible as part of the home health benefit: part-time or short-term skilled nursing care, physical therapy, occupational therapy, speech-language pathology services, social services, and part-time or short term home health aide services. There are certain requirements that must be met to be approved for the Home Health Benefit.
Who Qualifies for a Home Health Benefit?
In order to receive the home health benefit someone first have to be considered homebound. People who are homebound need help leaving their home due to being in a wheelchair, walker and/or crutches and need assistance from another person to leave the home. A professional must be the one helping and assisting with home health care. The patient must need care for a minimum of two months, and once a week for at least three weeks. The care can be extended but there are other requirements that need done in order for the extra care to be approved. Before someone starts their care at home, there has to be a one on one meeting with a physician up to three months prior to getting the assistance or a month after the assistance has begun. During this visit the physician will evaluate the patient and discuss all options and if it is determined that the patient will benefit most from in home care, they will sign off on what is called a home health certification and will approve of a care plan. During this one on one visit, the physician will determine if the patient is in fact homebound or not.
Whether the illness is chronic or temporary, someone can still be covered for services².The care plan that is drawn up between the patient and physician be recertified and needs checked every two months, but a physician visit is not required each time. If all someone needs is occupational therapy, Medicare will not cover Home Health Benefits. Also, the assistance needs to come from what is called a Medicare- certified home health agency³.
How Do You Start the Process to Get a Home Health Benefit?
Typically, this begins when someone is in a nursing facility or in the hospital. If someone feels like they need in-home care and help, all they need to do is bring it up to their physician and to discuss what options are available⁴.
What Part of Medicare Covers Home Health Care?
Both parts A and B of Medicare cover home health care but both parts cover it differently. Part B is the one that usually covers the home health care, but Part A will cover it too if there has been hospitalization involved. Part A will also cover 100 days of in-home care, but the patient still has to meet all of the other requirements necessary for the coverage. After the initial 100 days, Part B kicks in and starts coverage⁵.
Are There Things NOT Covered?
There is no coverage for having care all hours of the day, prescription drugs (because Part D covers that), home cleaning services, or services like Meals on Wheels, which is a service that brings food to the older adult’s front door⁶.
Since there is not coverage for all hours of the day, they allow assistance for eight hours in one day and up to twenty-eight hours in a week. In certain situations, there can be an allowance of up to thirty-five hours a week⁷.
References
- What’s Medicare? (n.d.). Retrieved from https://www.medicare.gov/what-medicare-covers/ones-medicare-coverage-choices/whats-medicare.
- Home health care for chronic conditions. (n.d.). Retrieved from https://www.medicareinteractive.org/get-answers/medicare-covered-services/home-health -services/home-health-care-for-chronic-conditions.
- Home health basics. (n.d.). Retrieved from https://www.medicareinteractive.org/get-answers/medicare-covered-services/home-health-services/home-health-basics.
- Starting home health care. (n.d.). Retrieved from https://www.medicareinteractive.org/get-answers/medicare-covered-services/home-health-services/starting-home-health-care.
- Eligibility for home health (Part A or Part B). (n.d.). Retrieved from https://www.medicareinteractive.org/get-answers/medicare-covered-services/home-health-services/eligibility-for-home-health-part-a-or-part-b.
- Services excluded from home health coverage. (n.d.). Retrieved from https://www.medicareinteractive.org/get-answers/medicare-covered-services/home-health-services/services-excluded-from-home-health-coverage.
- Home health hours. (n.d.). Retrieved from https://www.medicareinteractive.org/get-answers/medicare-covered-services/home-health-services/home-health-hours.