
Editorial Column By: David Wright, MS, PA-C, NRP
Emergency Medical Services (EMS) is an action packed, thrilling career that is packed full of explosions, gunshots and major traumas. Paramedics speeding to the scene, lights and sirens blaring, people are lying in the streets, screaming and crying when the medics jump out of the ambulance to save the day. Or at least that’s what the TV shows would have you believe. Watching any TV medical drama would have you believing that doctors are running out to the ambulance bay to meet dying patients who were impaled on a hiking trip, attacked by bears in the city or retrieved from an airplane wreck, but in my 15 years of EMS experience, this never seemed to be the reality of EMS.
Reality is more docile than the dramatic TV representation that gets good viewer ratings. According to a 2016 study, up to 50% of EMS transports are deemed inappropriate emergency calls for ambulance utilization.1 Most EMS workers would agree the current healthcare system in America is overworked and a visit to the emergency department will result in overcrowding of the waiting room, many of which are filled with patients not actually experiencing an emergency. It is important to have a clear delineation of two very different terms; unscheduled care is very different from an emergency. Emergencies are often life or limb threatening, while unscheduled care is just as it sounds, care that was not planned, but still care that needs to occur. Some attempts have been made to combat this with the recent proliferation of urgent cares, but let’s consider another possibility.
Many years ago, physicians would make house calls, but over the years, this model has gone away. Today there are still plenty of healthcare workers who spend their work day travelling from house to house, providing in home continued or preventative care. Many of these providers include home health nursing care, therapy services, social services, and EMS providers. What if we could do this for some of the unscheduled care that is currently overcrowding local emergency departments?
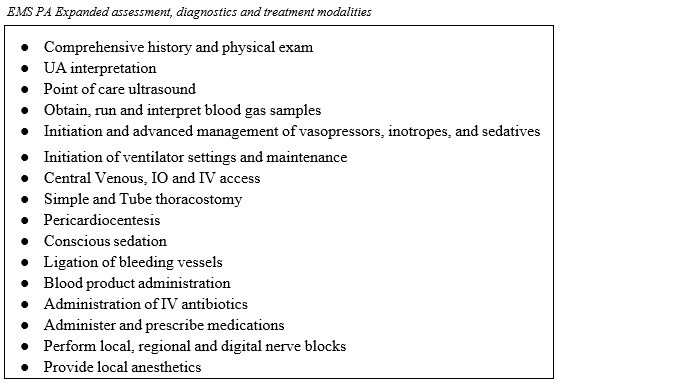
Physician Assistants (PAs) are well trained medical professionals who are capable of performing expanded assessments, can treat patients, perform and interpret laboratory data and prescribe medications.2 These qualities are currently missing from many of our pre-hospital care providers. In order to deliver well rounded, holistic EMS care, providers must be well versed in the unique challenges, interventions and situations that exist in the pre-hospital setting. A lot of this knowledge requires additional education not routinely taught in standard PA programs 6, enter the EMS Physician Assistant.
 Enter EMS PA Fellowships…
Enter EMS PA Fellowships…
To be able to care for this specific subset of patients in the pre-hospital setting, PAs, who are often trained in primary care medicine, would need additional education. That additional education should be focused in both the EMS and Emergency Medicine setting. The fellowship would include didactic work on core emergency medical conditions, assessment and acute management of these conditions, as well as appropriate disposition of patients who experience unscheduled care needs. Additional clinical hours and experience focusing on emergency medicine are also required. Standardized courses such as Basic Life Support (BLS), Advanced Cardiac Life Support (ACLS), Pediatric Advanced Life Support (PALS), and Advanced Trauma Life Support (ATLS) would be needed by the fellow. Additional Training focusing on common ED treatments for time sensitive diagnosis such as Stroke, STEMI, and Trauma would also be required. Skills training should also be included for procedures such as Central Line Insertion, splinting, immobilization, spinal immobilization, point of care ultrasound (with interpretation) and critical care hemodynamic monitoring would be provided.
 In addition to the core emergency medicine training, the EMS PA fellow would also need specific EMS training. EMS specific coursework includes Incident Command Systems (ICS), Emergency Medical Dispatch (EMD), and Hazardous Materials: Awareness level training. Specialized EMS training would focus on tactical medicine, mass gatherings, disaster medicine, urban search & rescue and fireground EMS care would also be completed. EMS systems also have administrative functions often performed or monitored by the Physician Medical Director. Training would also be provided to allow the EMS PA to be able to perform or assist in these functions, and education in QA/QI, continuing education, credentialing, and protocol development.
In addition to the core emergency medicine training, the EMS PA fellow would also need specific EMS training. EMS specific coursework includes Incident Command Systems (ICS), Emergency Medical Dispatch (EMD), and Hazardous Materials: Awareness level training. Specialized EMS training would focus on tactical medicine, mass gatherings, disaster medicine, urban search & rescue and fireground EMS care would also be completed. EMS systems also have administrative functions often performed or monitored by the Physician Medical Director. Training would also be provided to allow the EMS PA to be able to perform or assist in these functions, and education in QA/QI, continuing education, credentialing, and protocol development.

While cognitive education is important, it is equally important to have education in the psychomotor domain with practical hands on field experience. This experience would prepare the PA to work in the pre-hospital environment after graduation of the fellowship. Hands on field experience includes independent field response with local EMS providers, ambulance field experience, interacting with crews on scene, learning the EMS systems, participating in regional and nation exercises, and experiencing how EMS PAs integrate into the already established EMS system.
After Fellowship: What You Can Do On The Job
After graduation from the EMS fellowship and entering the workforce, the EMS PA would be adding an additional layer of pre-hospital care to the local and regional community. This addition would bring an EMS provider who is trained to provide adjunct services in critical care situations, tactical operations and community health. Including the high utilizers and the low acuity patients who primarily present with unscheduled care, rather than true emergency care needs. It is these patients that have the greatest potential to be dispositioned with on scene care and education, without the need for a hospital visit.
EMS PAs are capable of providing critical care by bringing additional tools and skills to patients who have experienced severe trauma, cardiac arrest or are involved in mass casualty incidents (MCIs). The capability of performing point of care ultrasound, advanced IV access, including central lines in critically ill patients to improve pharmacological resuscitation.3 Performing these exams in the field can improve patient outcomes by decreasing the overall time from injury to OR arrival.4 Patients who require extensive extrication due to entrapment or crush injuries can also benefit from critical care hemodynamic monitoring. EMS PAs are capable of inserting and monitoring arterial catheters for arterial blood pressure monitoring, or urinary catheters to monitor urine output and core temperature.
During cardiac arrests, point of care ultrasound imaging can confirm cases of cardiac standstill, a condition that drops the probability of successful resuscitation to essentially 0%.5 EMS PAs on scene can also provide on scene termination of resuscitation orders can also be provided in cases deemed futile by EMS PAs or on scene providers allowing responders to withhold/stop resuscitative efforts. Often families have more support at home to assist them through the loss of a loved one.
Mass gathering events such as Mardi Gras, special events, festivals, and state fairs brings another set of unusual challenges to a region’s EMS system. The EMS PA is capable of providing online medical control, giving direct orders, and operating outside of the usual paramedic protocols, to expand EMS provider capabilities on scene. These actions, include effective triage and treatment of patients can limit the amount of patients transported by ambulance to area emergency departments.
Police operations can be complimented by the addition of EMS intervention and training, and EMS PAs are able to provide a higher level of care for officers and potential patients when these situations arise. This EMS/law enforcement partnership can also strengthen the community cooperation and improve the law enforcement team health as the EMS PA is also capable of performing preventative care for tactical team members.6
 Many EMS systems are frequently plagued by high utilization users. Pre-hospital studies have demonstrated the possibility of almost a 50% reduction in these calls by providing appropriate patient education, resources and disposition to facilities other than the emergency room.
Many EMS systems are frequently plagued by high utilization users. Pre-hospital studies have demonstrated the possibility of almost a 50% reduction in these calls by providing appropriate patient education, resources and disposition to facilities other than the emergency room.7
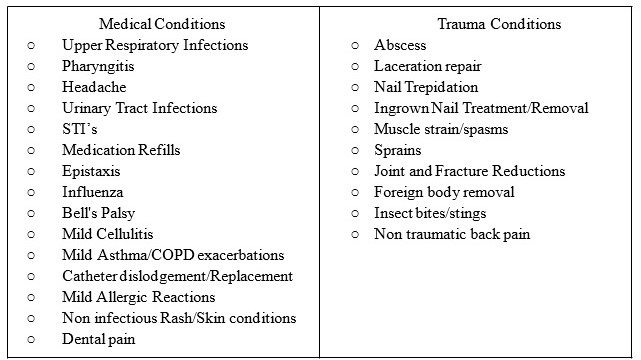
Paramedics also frequently encounter low acuity patients who are not experiencing a true medical emergency but rather have unscheduled medical needs. It is here the EMS PA may make the largest impact on the healthcare system. These patients are often potentially able to be dispositioned on scene as part of a “treat and release” program without needing medical transport. The following list of conditions are high frequency calls that have the potential of being dispositioned on scene without a hospital visit.
Conclusions
There are some small barriers to the implementation of a pre-hospital focused EMS PA post-graduate education program but considering the basic framework for the fellowship already exists, the program would be relatively easy to implement. PAs are already highly trained medical professionals who have the ability to improve and augment the current delivery of pre-hospital medicine. Attributes of a well-trained EMS PA increase assessment and clinical skills, improved resource allocation, decreased ED utilization, decreased healthcare costs, and improved overall health literacy.

References
1 Dejean, D., Giacomini, M., Welsford, M., Schwartz, L., & Decicca, P. (2016). Inappropriate Ambulance Use: A Qualitative Study of Paramedics’ Views.. Healthcare policy, 11(3), 67–79.
2 American Academy of Physician Assistants (2019). What is a PA. Accessed from: https://www.aapa.org/what-is-a-pa/
3 Bøtker, M. T., Jacobsen, L., Rudolph, S. S., & Knudsen, L. (2018). The role of point of care ultrasound in pre-hospital critical care: a systematic review. Scandinavian journal of trauma, resuscitation and emergency medicine, 26(1), 51.doi:10.1186/s13049-018-0518-x
4 Bloom BA, Gibbons RC. Focused Assessment with Sonography for Trauma (FAST) [Updated 2019 Jun 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470479/
5 Cureton, E. L., Ereso, A. Q., Sadjadi, J., & Victorino, G. P. (2008). QS243. The Heart of the Matter: Utility of Ultrasound of Cardiac Activity During Traumatic Arrest. Journal of Surgical Research, 144(2), 363–364. doi: 10.1016/j.jss.2007.12.490
6 National Tactical Officers Association (2018) Tactical Response and Operations Standards for Law Enforcement Agencies. Accessed from: http://ntoa.org/pdf/swatstandards.pdf
7 Clarke, J. L., Bourn, S., Skoufalos, A., Beck, E. H., & Castillo, D. J. (2017). An Innovative Approach to Health Care Delivery for Patients with Chronic Conditions. Population health management, 20(1), 23-30.doi:10.1089/pop.2016.0076

